Colten interacted with one of his feet today 🙂 This probably seems pretty silly to some of you, but it made me super excited! One of his goals that we set with EarlyOn, was that by 6 months of age, we want him to “know” he has feet, since he cannot really move or feel them. And when I pulled his leg up in front of his face today, he looked at it, reached out, grabbed at his calf, and pulled his leg towards his mouth, even getting his big toe in there for a second. It was all over in about 5 seconds but I was so excited in those 5 seconds, I almost cried! Now doing it once isn’t “proof” of anything – our PT at Mott told us if he can do something consecutively three times, it’s not random. I tried to get him to engage again but he seemed over it. Anyhow, screw the 3x rule, I’m still excited!!
We Finally Ran Out of Diapers!
When we brought Colten home from the hospital back in October, Richard was changing Colten’s diaper for the first time at home and in complete exasperation said, “We are never going to be able to leave him with anyone! We are never going to be able to go anywhere ever again!” At the time, we were so tired and overwhelmed that this comment did not feel all that far-fetched. Looking back on it now, it is, (as Parker would say) – “hilllllaaaarious. And I often remind Richard of him saying this!
The remark was due to the constant stooling Colten was experiencing. That, combined with the medications he had been on while in the NICU, caused his rear end to be so raw and sore that the Wound Care team at Mott had to come up with a butt paste regimen for diaper changes. It involved a three-step process of a few puffs of a powder-like substance to keep the area dry, followed by a spray-on barrier liquid that needed a minute to dry and harden, followed by a thick coating of cream. Attempting to do all of that before more fluids oozed out was frustrating. And messy. Inevitably, as soon as the fresh diaper was going on, it was getting soiled. But you cannot really change diapers every few minutes so the “triple threat” regimen helped protect his bottom while he sat in his own, well, you know.
After we came home, we had to continue applying the “triple threat” until his bowels calmed down a bit and his skin built up a bit more strength. As the medications finished coming out of his system, we were able to reduce the frequency of application and finally got to the point where we would just do it once or twice a week. Thankfully. He still stools quite often, there’s just not nearly as much medication creating havoc on his bowels. But at the time, it sure did feel like it would never end and we would never be able to have someone else do the process. I had, however, bought latex-free (a latex allergy is common in people with Spina Bifida) gloves in preparation of someone else having to do it. Because I couldn’t exactly ask someone to spread cream on my child’s behind while he continues to stool out of it, and then not provide them gloves!
What does this have to do with running out of diapers then? Because of the agressive creams we had to use with Colten, we knew coming home we would not be able to use cloth diapers, which we’ve used with our other sons. Creams get embedded into the diapers and prevent them from absorbing what they need to absorb *(see endnote). We love our cloth diapers – a lot (we use Rumparooz brand, in case you’re curious). We think they’re adorable, environmentally friendly, super absorbent, and better yet – we don’t have to keep spending thousands of dollars on diapers with each child. Spend a few hundred on diapers and we’re set for multiple kids for years! So when we realized we would not be able to use cloth, the added expense of buying disposables suddenly became very real. However, we had a great many people give diapers to Colten/us when we first got home. Not a great many people – a crazy great many people – SO many that Colten just turned five months old and WE FINALLY RAN OUT OF DIAPERS! Can you believe that we had THAT many diapers?! A HUGE thank you to those that gifted diapers… THANK YOU!
We are out of disposables and Colten rarely needs creams… So yesterday I re-snapped some of our cloth diapers down a size and put them in Colten’s drawer by the few remaining disposables (set aside for slightly easier travel days when needed). And I smiled as I remembered that first diaper change at home four and a half months ago…
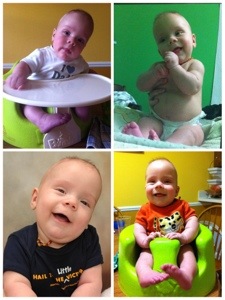
Happy boy sporting a cloth diaper

* Thanks to the recent information provided to us by the wonderful owner of Little Green Branches, a great eco-friendly baby & mom shop in East Lansing, we learned that we can actually use creams with cloth diapers if we put a thick enough liner down and wash the liner with our regular laundry, not our diapers! Yay! Also, a huge kudos to Little Green Branches as well for their professional diaper stripping service! No, this is not babies stripping out of their diapers – it’s a thorough cleaning process to rid diapers of smells, creams, and anything else “stuck” in the fibers. Highly recommend them!
Put Socks on that Kid! And a PT Update
The other day Parker told me, “I love Colten because he has purple feet and that’s my favorite color!” (And yes, that really is Parker’s favorite color!) It was both adorable and sad at the same time. Those of you that have been on our adventure may already have a sense of some of this, yet I’ll give this information again for new followers or as a reminder before I get further into today’s post…
Colten’s Spina Bifida defect is around L4 (we’ve been told L3-S1 by various medical professionals). He has strong quad (thigh) muscles, strong hip flexors, weak hamstrings and weak hip extensors. He appears to have some movement in the left lower leg as well – I don’t know this muscle name but basically he can ever so slightly, on occasion, flex his left foot upwards. He doesn’t push it back down and doesn’t seem to have any movement of the right lower leg. Sensation is a little hard to determine yet since he cannot tell us what he feels. We can (and do) pinch parts of his legs and feet and toes looking for a reaction from him, and assume that if we get three identical responses in a row to the same spot, he has feeling there and it’s not random movement. So the results are scattered and it’s not something we worry too much about at this point anyhow. With all the nerve issues that exist due to the Spina Bifida Myelomeningocele, blood flow is also reduced to the lower extremities. So his feet are often cool to the touch.
Why am I explaining this? Because his feet are always cold yet we rarely put socks on him and for some reason, I feel the need to explain WHY. Often times, putting socks on Colten means that either his feet will stink more or his feet will be even colder. The stinkiness, from what we can guess, is because his feet are trapped in warm booties and because he cannot move his toes, toe jam just collects in there and stinks up. The fact that his feet can get colder in socks seems to be from even the slightest extra pressure around the lower part of the leg – it reduces the blood flow that much more to the feet. So instead of being warm when we take socks off, his feet are actually colder! Why not just get looser socks? Because they just don’t stay on! His feet point inward and when he does move his legs around, his feet just kind of flop and hit the opposite leg and cause loose socks to just come off. So we just leave well enough alone. They aren’t FREEZING, even though they do look quite purple, as Parker noticed. And so when you see his chilly feet without socks, now you know why. Plus without socks, we can give stronger sensory input to his feet, just in case a nerve somewhere in there decides to wake up, or grow, or something!
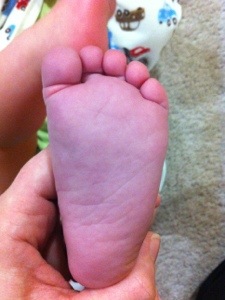
You can tell a little in this picture how purple his feet look… Coincidentally, Parker has on his favorite tshirt. Purple of course!

The next two show both the purple color, then the lack of circulation. Right before I took the second picture, I pressed on the bottom of his foot with my thumb. I waited quite a few seconds then took this picture. The coloring takes a while to come back.
Speaking of feet, onto a physical therapy update! EarlyOn continues to send us our wonderful PT, April, every two weeks. To the house. Have I mentioned how much I love this?! She usually comes when the other two boys are napping so it works out nicely to be able to do Colten’s appointment without interruption. Colten is 4.5 months old and is starting to sit with a bit of stability (hands in front of him for balance), keeps his head upright better, and can roll himself crudely from belly to back (easier roll). He is pushing up with his arms and trunk when on his belly and when given assistance with his legs and pelvis, can get his trunk and head to complete a back to belly roll (harder roll). She is very happy with those movements and the strength he is exhibiting in his trunk. All of those movements are age-appropriate. He is such a people-lover that he is far more interested in interacting with faces than toys. Not a bad thing, just a “noted” thing. And he is obsessed with his fingers in his mouth. So much so that between that and the people-loving, he has no need to unclench his hands, spread his arms, and grab at toys. This is a little behind the game in what she would like to see. He just doesn’t express much interest in doing anything with his hands except eating them. So we’ll continue to introduce some different textures to see what might entice him to open up those hands. So far he seems to enjoy crinkly baby books.
One of the things we spoke about at the appointment on Tuesday was sitting. As we’ve been working on that skill with him a little bit each day, I noticed that when sitting he really doesn’t move his legs at all and as soon as he tries to move more upright, he tips backwards and loses all balance. Watching him, something seemed different about how he tipped and I realized that when we are seated, legs out in front of us, and we tip back, we react by tightening our legs and digging our heals into the floor a bit. (Go ahead, try it, then keep reading…) Colten does not seem to have the muscle development (at least yet) to do this heal digging, so it is imperative that we build a strong, solid, balanced core to help him offset the unstable foundation under his trunk (the legs).
When Colten rolls from back to side, in preparation for rolling back to belly, often he gets his legs caught under each other, and as he attempts to roll further, he engages his muscles throughout his core. However, he also activates his hip flexor muscles, which pull the legs and knees upwards and prevent him from rolling further. So we need to work on helping him straighten those legs out flat so he can continue through the roll, and use his trunk to get his body over since his hips and legs aren’t helping to propel the motion.
Right now, we are very happy with how he’s developing. He’s on track for his age in most areas and even a little ahead in some others. We have a few things to focus on and we know it will get tougher as he gets older. We love where he is at right now though! It is funny how this is our third child and I feel like I am learning so much more about baby movement with him than the other two. Every move is dissected and evaluated. With the other two, we really didn’t teach them to roll or sit or crawl – they eventually just did it. Now, we have to step back and help his body learn how to move or adapt in smaller ways so that he can eventually learn how to do the larger movements himself.
Sympathy is Not a Strength Here
Most of our posts here really focus on Colten’s adventures, not our own random thoughts and processing. Although these posts do help us (or at least me – Colten’s Momma) process a lot of information. But today I’m straying a little from the usual type of post providing information about Colten, a therapy, or a diagnosis, to give you some insight into my own psyche. You’ve been warned. Read on with caution.
I was messaging with another mom today, a mom of a child with SB, and I said that if Colten’s bronchitis is our biggest issue right now, we must be doing ok! Then I remarked how Spina Bifida makes me see those other “normal” childhood illnesses in a whole new light. What’s a little bronchitis? No big deal! Right?!
We’ve never been a super-medical family. We do all that weird natural stuff that makes people raise eyebrows and probably talk about us when we’re not around. Our first two sons were born at a birth center with the help of midwives. We don’t usually give medication for ear infections. We amp up on certain homeopathic things when getting colds. We believe naturally immunity is good for the body. So to have even taken the boys to the ER the other night, or even to take Colten in for a cold, is way outside of our (prior version of) normal.
However, I have been a bit more neurotic about Colten – afraid that anything (spitting up too much, sleeping too much, not having “wet enough” diapers) could be a sign of something more – a shunt issue, a UTI, or some other issue I don’t know about yet. So I’ve been more neurotic, although not necessarily any more sympathetic. And even LESS sympathetic with the other males in the family (I say males, not boys, because Richard is included!).
The other day, Parker scraped his toe on something in the basement and according to Richard was absolutely fine after it happened. Until he sat down and saw one teeny-tiny drop of blood. Then the screaming and crying came flooding out! A bandaid was of urgent necessity and tears were flowing. Typically when my children get injured, I am quick to help calm them yet try not to baby them through it. Those that know me know I’m not uber-sympathetic. And it was worse before kids. Suck it up. Move on. When Richard complains about something my response is often, “Well, what are you going to do about it?” When the kids need a bandaid removed, I rip them off quickly, I don’t gently tear back (although I did make my Aunt-in-Law remove Colten’s head bandage when he had his shunt placed the first time). So sympathy just isn’t one of my strengths. Mean Momma.
Now, these little bumps and bruises the kids get have me being less sympathetic. And honestly, slightly annoyed at the dramatics. And doing a lot of wondering. I get that Parker, at almost four, is more aware of his body, gets what blood is, and it scares the crud out of him. And, again, he’s barely 4. I really need to remember that point. But I see him breakdown and (horrible mom admission coming…) think, “This is NOTHING compared to what Colten has gone through – and will go through. Suck it up!” Don’t worry – I do not say that out loud! And I feel guilty afterwards for even thinking it. Then I start to wonder – every single time, what Colten will be like when he’s 3 and gets injured. Or when he’s 2 and has to deal with another hospital stay. Or has to be catheterized. Will he be so used to medical stuff that he will take it in stride? Or will he scream and fight and resist anything being done to him (much like our last urology appointment)?
One thing I do realize during this all is that right now we actually have it really good compared to many families out there managing cognitive issues, life threatening diseases, other severe birth defects, and more. We are fortunate that the extent of Colten’s medical adventures are mostly physical in nature. And you know, four month olds don’t really do a whole lot physically anyhow! On that note, watch for an update on Colten’s physical therapy in the next day or two…
And for the picture fans out there, here is one of the boys from today at our favorite coffee place, Biggby! They enjoyed a special treat of hot chocolate and donuts. Not at all healthy or natural 😉
Because “Just a Cold” Would Be Too Easy
The older two boys have been sharing cold germs generously over the past week, so it is no surprise that Colten eventually started coughing, sneezing and sniffling. We were at the doctor today to followup on Parker’s ear infections, Max’s wheezing, and to let the doctor take a look at the newly symptomatic Colten (and to have his “creaking” checked out – maybe another story for another day?!). Thankfully, our wonderful nanny, Chelsea, who is with us three days a week, was available to help trek the boys with me!
The older two boys checked out fine. But apparently, as my sister Sarah put it, Colten “must have been bored.” The doctors heard quite a bit of noise rattling in his lungs and gave him a breathing treatment there in the office. He sounded a little better afterwards and was prescribed breathing treatments at home four times per day as needed.
He’s just trying to keep us on our toes. Make sure we don’t forget about him. Like we could forget about this cutie..

Tummy Time, Rolling, and Other Baby Stuff
Sometimes I have to remember that Colten’s adventures include not just his medical experiences but also the normal child development progressions!
This week, our EarlyOn PT, April (we really like her – she is great!), worked with Colten on starting to feel his body roll over, sit up, and grab at toys. He isn’t necessarily behind in these stages – a little delayed on grabbing at toys because his fists were clenched for so long due to the hydrocephalus and still stay clenched quite a bit, but rolling over he still has some time to work towards. Usually by about 6 months on average is when babies tend to roll back to belly, with belly to back coming sooner. Sitting up unassisted usually occurs around that 6 month mark as well.
Seeing that Colten wasn’t yet grabbing for any toys, April inquired as to what all Colten was getting exposed to holding or grabbing at these days. I told her that the only thing he seemed to grab and pull up to his mouth to explore was if I left a burp rag on his belly or in front of him on the Bumbo. He seemed to not have any interest in any rattle, ring or other toy we showed him. April suggested a crinkly toy and I dug a book out of the boys’ book basket that has touch-and-feel pages of animals as well as a crinkly front cover. Well that was all Colten needed! He loved it. He enjoyed scrunching it up, eating it and even enjoyed some tummy time with the book. Time to go digging for some more scrunchy toys!
Speaking of tummy time, we are not big pushers of it so this is really the first week that Colten has had significant tummy time and he’s already four months old. Most of his tummy time is actually tummy-to-tummy time on Richard or me, as we lean back on the couch with him. While tummy time is something that helps babies develop neck strength and use both gross and fine motor skills, I find it funny that both the AAP and Mayo Clinic push the fact that tummy time helps avoid a flat spot from babies laying on their backs too much – which they also both say is not a developmental concern, just a physical appearance “problem”. So this has never been as big of a concern for us since we actually tend to wear our kids in wraps and carriers as opposed to leaving them laying on the floor – babywearing also avoids misshapen heads! And even in the carriers, as Colten stretches himself upgright when looking around, he will push with his arms against me to move his body, strengthening his arms. The upright position of the carriers also helps build neck strength, just as tummy time would (and of course back-lying does not). Also, since tummy time does put a lot of strain on the spine, I was particularly cautious of it with Colten due to the trauma to his spine from the spina bifida myelomeningocele and repair. So to be honest, he really hasn’t spent more than 1 minute at a time on his belly until the last two weeks. The reassuring thing for me was that as he’s on his belly now, he’s totally content and happy (NOT the case weeks ago!). So I feel more comfortable that he is ready for tummy time. AND after just one little session of encouragement from April on rolling belly to back, Colten can do it on his own now when he’s done being on his belly. Another sign that he truly is ready for tummy time!
Looks pretty happy to me…
Kidney APPEARANCE and Kidney REFLUX are Different.
You would think this is an obvious thing, right? How your kidneys measure and appear on an ultrasound isn’t the same as how they function and process our bodily fluids. Makes sense. Apparently yesterday, I assumed one meant the other. In other words, yesterday’s post claiming “no more reflux” was a lie. All lies.
So here’s what kidney reflux is, in case I haven’t explained it before:
Vesicoureteral reflux is the abnormal flow of urine from the bladder to the upper urinary tract. The urinary tract is the body’s drainage system for removing wastes and extra water. The urinary tract includes two kidneys, two ureters, a bladder, and a urethra. Blood flows through the kidneys, and the kidneys filter out wastes and extra water, making urine. The urine travels down two narrow tubes called the ureters. The urine is then stored in a balloonlike organ called the bladder. When the bladder empties, urine flows out of the body through a tube called the urethra at the bottom of the bladder.
In VUR, urine may flow back—reflux—into one or both ureters and, in some cases, to one or both kidneys. VUR that affects only one ureter and kidney is called unilateral reflux, and VUR that affects both ureters and kidneys is called bilateral reflux.
(taken from the National Kidney and Urologic Diseases – Information Clearinghouse (NKUDIC))
Colten has bilateral reflux. It is classified in severity by grades 1 through 4, with 1 being most severe and 4 being least severe – Colten’s is grade 2. I swear at some point I read it was 3/4 but apparently I’m just full of lies these days because the last two documents I just double-checked say “grade 2”. It is something he may outgrow over time, although they will not retest him for it until about one year of age. Silly me – I thought the renal ultrasound was the check, but that’s only part of it. The ultrasound did show that his ureters are continuing to grow and develop, and that they are not being negatively impacted by the reflux at this point. To check if the reflux is still occurring, a VCUG, or voiding cystourethrogram, must be done.
VCUG is an x-ray image of the bladder and urethra taken during urination, also called voiding. The bladder and urethra are filled with a special dye, called contrast medium, to make the urethra clearly visible. The x-ray machine captures a video of the contrast medium when the child urinates. The procedure is performed in a health care provider’s office, outpatient center, or hospital by an x-ray technician supervised by a radiologist—a doctor who specializes in medical imaging—who then interprets the images. Anesthesia is not needed, but sedation may be used for some children. This test can show abnormalities of the inside of the urethra and bladder.
(taken from the National Kidney and Urologic Diseases – Information Clearinghouse (NKUDIC))
Reading more on the website linked above though, an abdominal ultrasound can also be used to test for reflux so you can be sure I’ll ask for that over the x-ray when the time comes. One of you will remind me, right?!
This all started came to light when I called the nurse line today to ask if we could take him off his meds since the reflux was gone. The nurse was quite confused as to where I got that information from. And it was the same woman that had attempted to cath him yesterday. So I’m sure she thinks I’m a bumbling idiot for 1-not being able to console my child and 2-making up what the doctor told me. She informed me that Colten does need to continue his daily preventative dose of antibiotics to keep the UTIs away. From what the NKUDIC site says, “When a child with VUR gets a UTI, bacteria can move into the kidney and lead to scarring. Scarring of the kidney can be associated with high blood pressure and kidney failure. However, most children with VUR who get a UTI recover without long-term complications.” She also informed me that maybe for his next cystometrogram, I can try to wait a bit to feed him and then feed him on the exam table, if I’m comfortable with that. Yes, I believe I’m comfortable with that!
We still go back in three months to attempt the cystometrogram again that they couldn’t do yesterday, and he’ll get a VCUG (or ultrasound instead!?) at around one year of age.
Sorry for the lies yesterday – I blame it on the crying kid. I think my head was in a fog because of that and I just heard what I wanted to hear! Colten and his chaos. Maybe THAT should have been the name of this blog. Hm. Not very nice, no. We’ll leave it as is.
Urology Fun Day
This post’s working title was “More Weird Places I’ve Breastfed My Children”. Sigh.
Warning: this post talks a lot about breastfeeding, bladder function and bowel function. If you’re uncomfortable with any of these, please stop reading. There are also not many pictures today seeing as the topics are what they are 😉
This afternoon I trekked to Mott with my three little boys, leaving Richard to enjoy some science classes at LCC and MSU. Next time I’ll trade places with him. Thanks to our wonderful friend Brynn, Parker and Max got to spend a couple hours at the Ann Arbor Hands On Museum (thanks Brynn!) while I took Colten to his appointments. Today he had his follow-ups with the pediatric urologist, Dr. Wan.
[Fireman Parker and Fireman Max at the Ann Arbor Hands On Museum]

His first appointment was a renal ultrasound. When Colten was born, one of the diagnoses we received in addition to the Spina Bifida Myelomeningocele, was bilateral kidney reflex. My understanding of this is that urine backs up from the bladder through the ureters and back to the kidneys. The grade (severity level) of his reflux was on the lower end and the doctors hoped he would simply outgrow it. Otherwise, surgery would be needed to correct the issue. Hence the renal ultrasound today.
[In case you haven’t read all of our posts here, bladder and bowel issues are pretty much universal for people with myelomeningocele. The bladder and bowel nerves are at the base of the spinal cord and since everything associated with the spinal cord nerves at the area of defect AND BELOW are typically affected, even the lowest level of myelo, the sacral regions, will deal with bladder and bowel issues. Colten’s level of defect is lower lumbar, around L4-L5.]
So Colten has had 12 ultrasounds over the past four months (cranial, hips, spinal, renal) and has usually cooperated quite well. The early ones while in the NICU, he mostly slept through. Our followup ultrasounds since then have gone smoothly. No fuss. He just lays there and cooperates. Until today. My oh my. As soon as I laid Colten down on the table the screaming began. In his defense, he had just started nursing in the lobby when I had to interrupt him because he was called back for his appointment. So as he fought and fussed for the ultrasound tech, I said to her, “If you are okay with it, can I just lean over and finish feeding him? Otherwise he’s going to just continue screaming.” She was fine with it and so I attempted to pacify him while the tech continued the ultrasound. Well, Colten wanted NOTHING to do with this arrangement and continued wailing. I asked her to stop again so I could try to console him. She asked if I could try laying down on the bed with him and he could nurse side-lying while she did the ultrasound on his back instead of his belly. Nope, Colten wanted nothing to do with laying on that bed whatsoever. He continued to scream – tears flowing, mouth quivering. I picked him up, held him close, rocked him and settled him down. We ended up having to do the ultrasound that way, which worked out fine. End result? No more kidney reflux! Hooray for Colten! I am hoping that this means he can also come off the antibiotics, but in the commotion of today, I forgot to ask. I’ll make that phone call tomorrow for sure! [UPDATE: Kate had her information skewed a bit. Please be sure to read the NEXT post for an update.]
Onto our second appointment, the cystometrogram. This procedure requires catheterization. Once catheterized, they fill the bladder and then measure how it empties. It is common for some people with myelo to not empty their bladders all the way. This creates a host of issues so catheterizing is often needed multiple times a day for life. I’ll skip the description of watching the first staffer attempt twice to cath Colten. Unsuccessfully. REALLY?! Meanwhile, Colten is not a happy camper. He started fussing as soon as I laid him down on the table again and not surprisingly, screamed throughout the attempts at cathing him. She finally went to get Dr. Wan so he could cath Colten. After that was done, she informed me that if Colten couldn’t calm down, she wouldn’t be able to do the test. In order to get the readings, Colten would need to be lying down and not agitated. Here we go again. He is screaming, crying and inconsolable. At this point, I am fighting back tears because I’ve watched these people shove a tube up my son’s private parts, had to hear him scream throughout this all, watch tears come out of his eyes, and I could do nothing to help. As he is laying on the exam bed, I’m trying to calm him but cannot use any of my normal ways at this point… Colten really isn’t a fussy baby and is usually easily calmed by nursing or just being picked up and held or worn in a wrap/carrier. But he has had 2 of these all-out screaming episodes before and we just have had to ride them out, holding him and getting him to sleep.
However, Colten is naked and with his bowels, he is almost constantly stooling. So by now, with all the crying he’s done, the blue pad he is laying on is a mess with poop. So I can’t quite get him picked up. Finally the staff member (still have no idea if this woman was a nurse practictioner, doctor, aide or what) asked me to try sitting on a chair by the test equipment and trying to nurse him to calm him down. She put a blue pad on my lap and I cradled him in my arms and tried to nurse him. So another weird nursing experience in the books. Anyhow, it didn’t work and she couldn’t do the test. Catheterized for no reason. Poor boy. We have a repeat of this test scheduled for May. For now, we have to monitor for enough wet diapers and watch for UTIs.
So we got some good news in that the reflux is resolved. No bad news yet in regards to having to cath. And I added two new weird nursing experiences to my list. Oh, you haven’t seen my list? Well, I’ll spare you all the details. Let’s just say my experiences with Colten include nursing while standing and leaning over the side of his NICU bed, nursing during one of his physical therapy stretch sessions, and nursing during part of one of his Anat Baniel Method appointments. Ah, the quirks of breastfeeding!
Here’s Colten soothing himself in the car as we get ready to head home… We’re hoping the finger up the nose while sucking on other fingers won’t be a habit. But he sure does love his fingers!

Development of the Nervous System in Spina Bifida
At Colten’s follow-up cranial ultrasound today, Dr. Maher was pleased at the functioning of the shunt and the levels of fluid in Colten’s ventricles. So we got a thumbs up and as long as all continues to progress this way, we will not need to see neurology for another six months. YAY! That seems insanely crazy considering we’ve had 5 appointments with neurology over the past 3 months, not including the daily appointments with them while Colten was in the NICU and then while he was in the hospital for his shunt and revision. So to not see them for six months is going to be a bit odd. Even during our mini-breaks from medical appointments (most of December!), we get kind of lost in the day to day of life (a good thing!) and forget that there is a whole future of challenges ahead. This is nice because it lets us just enjoy what we have right now and not have to think of the things that have not hit us yet (some days; other days, honestly, I obsess wondering when X, Y or Z is going to happen). So hooray for not seeing neurology for six months!
Since there wasn’t much to discuss at the appointment with Dr. Maher, I attempted to get clarification on how exactly a child with myelomeningocele develops his/her nervous system compared to a child without myelo. In my elementary knowledge of the spine and nerves, I see a great big thick cord going down the back with smaller off-shoots coming out of it, and even smaller ones out of those, and on and on until you get to the microscopic nerves that help us move our fingers, feel a rough surface, react when a stove is hot, etc., like the root system of a tree. So from what I understood about myelomeningocele, I was picturing the spinal cord looking quite the same, except that the ends of the “roots” just didn’t grow all the way and didn’t get down to Colten’s feet. They fell short or went elsewhere or got lost in the cyst on his back or just did not form at all.
According to Dr. Maher, and I won’t quote him exactly because frankly my memory isn’t that good and I don’t want to credit him with something that maybe I didn’t understand or maybe misinterpreted, but here’s the gist of what I got from his description:
The nerves don’t all grow out from the spine like roots of a tree. Yes, the spine does have many nerves that grow out from it, but they connect with nerves coming in from various body parts. In utero, the feet grow “foot nerves” and in normal development, these foot nerves find and connect to the nerves coming out from the spine, making synaptic connections. When you have this type of defect, the nerves are present all over the body, but they aren’t all making connections to each other. Coming out of the very base of the spinal cord are the nerves that control bladder and bowel function, and in myelo, these nerves are almost entirely missing or defective. As you move up the spine, the nerves are all very different from myelo kid to myelo kid. So yes, he has nerves in his feet most likely, but they are not making connections to the nerves that came from the spine – either because the nerve from the spine simply didn’t develop, or is damaged. There is also a poisoning of the nerves due to the exposure to amniotic fluid. So even when a nerve is physically there, it could be damaged that way.
Dr. Maher went on to explain that these kids have gaps in their nervous system. In utero, if the nerve formed but didn’t make it to where it needed to go, it wasn’t being communicated with. The foot wasn’t getting any signals from the spine/brain so it wasn’t moving and it wasn’t providing any neurological feedback back to the spine either. After a while, that nerve just became unresponsive. It’s dead. That’s why we see less muscle development in the lower legs with these children. The nerves were not being communicated with so they didn’t help move the leg and build muscle.
Relaying this information to Richard, he became quite excited because the fact that there should actually be nerves in Colten’s lower extremities is a big plus on our side and makes the Anat Baniel Method even more appealing. ABM works on making connections between the body and the brain. But it certainly needs nerves present to do this. The connection needs to be from the body part to the nerve to the spine to the brain. However, my hesitation still exists because we don’t know how big that gap is between the foot nerve and the “buddy nerve” coming from the spine. And we don’t know how big of a gap can be overcome. And we don’t know if the buddy nerve is even functional or present. So there are still a lot of big IFs out there. But it certainly seems more viable as an option to create better connections for Colten to one day use his lower legs and feet more effectively. We’ll take that!
Colten, Untipped
Sunday night I was taking some pictures of Colten and realized he was holding his head completely differently than before.
[PLEASE NOTE: The Bumbo seat, for those that have not heard of it, is an infant seat that has been recalled at various times by the manufacturer after families filed complaints of their children falling out of it. We continue to use this molded foam seat in a safe, supervised manner according to the manufacturer’s instructions, except we do sometimes use it at our kitchen table when an adult is sitting with the child, which is actually against the manufacturer’s recommendations; they say not to use on an elevated surface. If you are anti-Bumbo-use, please do not read further!]
So I noticed Colten was holding his head very straight up. Since he keeps trying to do sit-ups in our arms to be more upright, I had pulled the Bumbo seat up for him to sit in. We had tried it a few weeks ago and he just wasn’t strong enough yet. But on Saturday, Colten had another ABM (Anat Baniel Method) therapy appointment. This is what I consider his “neurological” therapy in a way. As opposed to “physical” therapy. And then all of a sudden, Sunday he is holding his head up straight and tall!! The PT, Richard and I have been trying to work on this leftward tip with stretching and strengthening exercises and he remained tipped to his left until now! It seemed awfully sudden and drastic, so I’m really thinking this had something to do with the ABM.
Here he is super happy in the Bumbo, along with three pictures from the previous couple weeks where you can see clearly how tipped he was prior to this weekend.
Note that the upper right picture is taken from a mirror so it looks like he is tipping the other way. He is not 😉