We have some appointments down at Mott Children’s in the next couple of weeks – follow-ups with Pediatric Neurology and Pediatric Urology. So before another round of medical posts, here’s just an update on life in general.
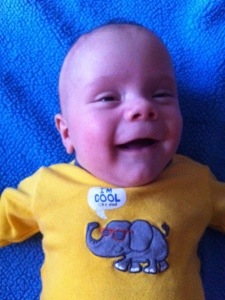
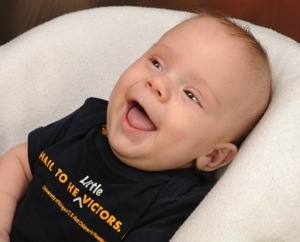
Those of you that know us know that our family leans a little to the MSU side of things – both Richard and I are graduates of State. Well, leaning a little is putting it lightly really. My husband bleeds green. However, with the University of Michigan C. S. Mott Children’s Hospital being the place that fixed up our little guy, Richard actually donned a maize U of M shirt while we were there, and bought the whole family matching shirts! The statement on the front says, “Hail to the Little Victors”. Here is Colten happily showing his off:
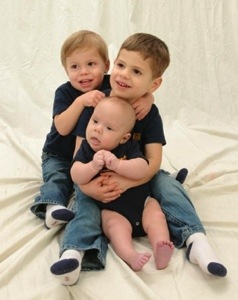
Colten is doing great and just enjoying the luxurious life of a three-month-old… Sleeping, playing in play yards, swinging in swings, nursing, spending time in baby wraps and carriers, having two older brothers in his face…
He continues to get EarlyOn PT every other week, Anat Baniel Method therapy will now be every week, and treadmill work every day – plus assessments every other week from the treadmill study team. And tons of other lovin’ from us! We even had a dear friend introduce us to Brain Gym too, so now while playing we incorporate some Brain Gym work. Mostly just moving arms and legs across the body. We even received some input on this from our Anat Baniel practicioner, Bethany. She encouraged us to do the Brain Gym movements in more random movements, since random movements are what babies do naturally to learn about their body, and to take the movements slowly and not pull past resistance. From what I understand so far, this cross-midline experience is very stimulating and challenging for the brain and can benefit children and adults of all ages and development ranges. She also informed us that the area of the brain that controls the hands is close to the area that controls the feet. So any stimulation we do to hands we should follow with foot stimulation to help try and make connections. I am still unsure about some of this since it seems pretty unclear whether the nerves Colten has even go to his toes, etc… But we are open to trying to give him the best shot possible.
We have not seen any other changes in movement. Colten has strong quadricep (thigh, or front upper leg) muscles. He seems to have some hamstring (back of upper leg) muscles and inner thigh muscles. He is not displaying lower leg movement (ankles, feet, toes), except an occasional upward pull, or flexion, in the left foot. I state this again as we have been to a few gatherings recently where people are surprised that he is moving his legs. Yes, he does move them! His lower leg appears to be moving, and even his feet “move”. But they move as an extension and result of his upper leg muscles. The feet flop wherever due to the movement of the rest of his leg. Hip and gluteus (butt) muscles control much of the upper leg movement. Upper leg muscles control much of the kicking, pushing, and pulling in of the lower leg. Lower leg muscles control the rotation of the lower leg and the ankle. That is what he seems to be missing. And no toe control either. Hopefully that makes sense. I will work on video taping this more clearly soon.
The rest of today’s post is just some Colten cuteness to enjoy!
Video of Colten loving on himself in the mirror.
Okay. Totally kidding. He’s not listening to anything and he doesn’t wear shoes while doing treadmill work. Here’s a real video of how he actually is on the treadmill!
Myelomeningocele Treadmill Study
That’s it! I’m sure we will be around again with updates over the next couple of weeks.